
Biomedical waste is highly hazardous which can give birth to serious diseases that may be lethal; therefore it is a problem of global nature. Biomedical waste management is of prominent importance to lessen the serious health consequences.
Introduction:
Biomedical waste is any type of waste either solid or liquid comprising of harmful materials produced by healthcare facilities e.g. hospitals, practices, health camps etc. This waste comprises of human tissues, contaminated blood, body fluids, discarded medicines, drugs, contaminated cotton, dressings, and sharps such as needles, glass, blades, scalpels, lancets. Biomedical waste collection and disposal has highest risk to healthcare, sanitation workers and the general community. The biomedical waste minus appropriate disinfection leads to acquired immune deficiency syndrome (AIDS), Hepatitis B & C, severe acute respiratory syndrome (SARS), tetanus, psychosocial trauma etc. Biomedical waste management is significant to defend the environment and health of the population.
Necessity of Biomedical Waste Management:
Inadequate management of waste produced in health care facilities causes a direct health hazards on the general public, the health care workers and on the environment. There is an obligation for the supervision of biomedical waste to abate the risk of contamination outside the hospital for waste handlers, scavengers and those living in the locality of hospitals. Management is also required due to the risk of air, water, and soil pollution, or due to unsuitable incineration emissions and ash. It plays a vital role in removal of the discarded drugs that can be repacked and traded off.
Biomedical Waste Management:
Biomedical waste management is of prodigious impact because biomedical waste can harmfully affect health leading to serious implications to the people who get in touch with it. Segregation, storage and safe disposal of the waste is very crucial to the effective management of biomedical waste in a workplace.
Segregation of Biomedical Waste:
Segregation of waste plays a chief role for enhanced biomedical waste management. It is imperative to decrease the volume of infectious waste or else the quantum of waste will go beyond the control of management. The waste is separated according to various colour coding system of waste containers which is given below:
- Red bag: Recyclable contaminated waste such as bottles, intravenous tubes, catheters, urine bags, syringes and gloves.
- Yellow bag: Human and animal anatomical waste, soiled waste including items contaminated with blood, body fluids like dressings, plaster casts, cotton swabs, expired or discarded medicines, chemical waste (liquid), rejected linen, mattresses, beddings infected with blood or body fluid, microbiology, biotechnology and other medical laboratory waste.
- Black bag: Incineration ash and chemical waste (solid).
- White bag: Waste sharps including needles, scalpels, blades, or any other contaminated sharp object that may cause puncture and cuts.
- Blue bag: Metallic body implants and glassware such as medicine vials, ampoules.
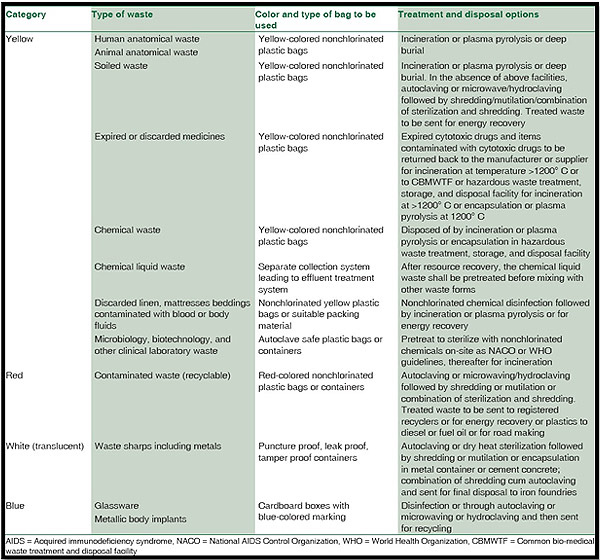
Biomedical waste classification – categories, treatment, processing, and disposal options
Storage of Biomedical Waste:
Healthcare facilities must make available a storage area for medical waste until it is collected for treatment and clearance. Storage area should be designated carefully which is remote to the general public and must display cautionary symbols & signs. It should be deposited in a dry and secured area before being transported. The area must be sheltered from water, wind, rodents, insects and animals. Harmful biomedical waste should not be stored for more than 3 months.
Treatment of Biomedical Waste:
Biomedical waste treatment refers to the procedures to eliminate the harmful effects of the waste. There are numerous treatment options which maximize safety during management and disposal of the waste. It also reduces environmental hazards. Incineration, Autoclaving, irradiation and chemical treatments are the most used methods for management and cleansing of biomedical waste.
Incineration
It is a treatment process used to transform pathological and pharmaceutical waste into ash, flue gases and heat. Functioning temperature for incineration should be in the range of 800-1400 degree Celsius. It reduces the bulk of waste by 90-95% and thus decreases harmful effects on the surroundings.
Autoclaving
It is a method of steam sterilization and is the most common substitute to incineration. Autoclaving necessitates a temperature of 121 degree Celsius and pressure of about 15 pounds per square inch (psi) for 20-30 minutes. This action is applied to inactivate the contagious agents and to sterilize the apparatus used in clinical services. It is less expensive and carries no recognized health impacts.
Chemical treatment
This treatment is frequently used to decontaminate liquid waste, so that it can be disposed-off nearby. It makes use of a number of techniques such as oxidation, reduction, precipitation and pH neutralization to transform waste into less dangerous substances. Chlorine, sodium hydroxide or calcium oxide can be used agreeing to the nature of waste.
Irradiation
These methods are at present being used in waste treatment procedures which include gamma, electron-beam, ultraviolet and X-rays. Irradiation sterilizes waste in a sealed off chamber by uncovering it to a radioactive cobalt-60 which gives out gamma rays that are lethal to micro-organisms. It is very costly as associated to other methods and protections must be taken to guard workers from detrimental effects of radiations such as cancer, radiation sickness or even death.
Disposal of Biomedical Waste
Land disposal is usually employed for remediation of waste which is decontaminated by appropriate treatment approaches. This technique is generally used in developing countries which includes the throwing away of waste into a landfill. Land-filling should be conducted at places where groundwater level is low and which are far from flooding sources. Radioactive wastes are commonly dumped in the oceans far away from human inhabitations. Every state and local government has its own rules and regulations for dumping of sanitized waste.
Advantages of BMW Management
Scheduling the waste management and reconditioning for all of the waste generated in the health care facilities is a fundamental task which plays an extremely significant role in the global cleanliness, public health, preservation of resources and sustainability of the ecosystem. Recycling medical waste curtails utilization of raw material and decreases the amount of the waste materials that must be disposed in a landfill. It decreases the dangers and risks to the communities which can be at risks due to hospitals. Decrease in the incidence of HIV/AIDS, sepsis, hepatitis, and other diseases spread by infectious medical equipment takes place by accurate waste management. Illegal trading of used syringes, injection needles and medical tools can also be stopped by proper management tactics. Attentiveness about perils of biomedical waste and its appropriate disposal is compulsory for a nontoxic and vigorous future.
Biomedical Waste Situation in India
In July 1998, first BMW rules were informed by Government of India, by the erstwhile Ministry of Environment and forest. In India, BMW problem was further aggravated by the existence of scavengers who sort out open, isolated health-care waste with no gloves, masks, or shoes for recycling, and following, reuse of syringe without proper sterilization.
During 2002–2004, International Clinical Epidemiology Network investigated the existing BMW practices, system, and structure in primary, secondary, and tertiary health care facility (HCF) in India across 20 states. They established that around 82% of primary, 60% of secondary, and 54% of tertiary HCFs in India had no trustworthy BMWM system. In 2009, around 240 people in Gujarat, India contracted hepatitis B resulting from reuse of unsterilized syringes. This and many more studies shows that despite India being among the first country to start measures for safe disposal of BMW, there is an critical requirement to take action for solidification of the existing system capacity, increase the capital funding and obligation toward safe disposal of BMW.
The BMW 1998 rules were improved in the following years – 2000, 2003, and 2011. The draft of BMW rules 2011 stayed as draft and did not get reported because of lack of consensus on categorization and standards. Now Ministry of Environment, Forest and Climate change in March 2016 have revised the BMWM rules. These new rules have amplified the coverage, simplified the categorization and authorization while refining the segregation, transportation and disposal methods to reduce environmental pollution. It has four schedule, five forms and eighteen rules.
Conclusion
Waste generation should be curtailed for the protection of environment and overall public health. People must be alerted to the issues connected to biomedical waste and should contribute in the programs structured for waste minimization. The medical employees must be taught to create alertness and foster accountabilities for inhibition of exposure and unsafe disposal to the waste. Medical personnel should rigorously follow all the rules and regulations instigated by concerned governing bodies.
BMWM should be a collective teamwork with dedicated government backing, worthy BMW practices tracked by both health-care workers and HCFs, continuous monitoring of BMW practices, and resilient legislature. It is our essential right to live in clean and safe environment. The pillar of BMWM is separation of waste at source and WR. The current BMWM 2016 rules are an advancement over earlier rules in terms of upgraded segregation, transportation, and disposal methods, to reduce environmental pollution and make certain of the protection of the staff, patients, and public. Moreover, more use of non-PVC medical apparatus and improvement of newer innovative, eco-friendly systems for disposal of BMW should be heartened. All contributors in BMWM should pledge to assure a cleaner and greener environs.
